Popular Reads
Top Results
Can't find what you're looking for?
View all search resultsPopular Reads
Top Results
Can't find what you're looking for?
View all search resultsRise of antimicrobial-resistant superbugs
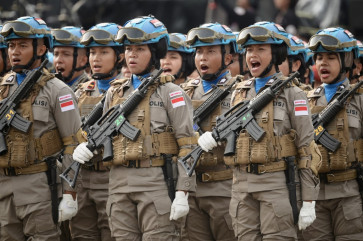
Spot check: Members of a joint operational team from the Jakarta office of the Food and Drug Monitoring Agency (BPOM), the Jakarta Police and the Jakarta Health Agency examine medicines for sale at a drugstore in Pramuka traditional market in East Jakarta
Change text size
Gift Premium Articles
to Anyone
S
span class="caption">Spot check: Members of a joint operational team from the Jakarta office of the Food and Drug Monitoring Agency (BPOM), the Jakarta Police and the Jakarta Health Agency examine medicines for sale at a drugstore in Pramuka traditional market in East Jakarta. The raid, held recently, was a follow-up to the discovery that fake and expired vaccines and drugs were being sold to the public.(JP/Donny Fernando)
The unchecked use of antibiotics in Indonesia and other developing countries has led to the emergence of antimicrobial resistance, a major global, and largely overlooked, health issue. The Jakarta Post’s health correspondent Hans Nicholas Jong provides an overview of the issue that will be addressed at the UN General Assembly high level meeting this Wednesday.
You accidentally cut your finger while chopping a shallot. Not a big problem, right? Just put a Band-Aid on your finger and you are good to go. But imagine a world where a small cut to your finger could leave you fighting for your life.
What if the most basic surgeries, like having your appendix removed, became deadly, and cancer treatments and organ transplants could kill you?
It seems like a plot from a science fiction novel. But those scenarios could become the reality in the near future as the world heads back to a time when antibiotics had not yet been invented: the medical dark ages.
Ironically, it is your penchant for using antibiotics that is bringing this post-antibiotic world into being.
Have you ever been in a situation where your cough will not go away? Having a hard time getting rid of your runny nose? Chances are you will be tempted to go and ask your doctor if they can give you anything for it.
Often that “anything” will be antibiotics as they are regarded as a cure-all. After all, antibiotics are certainly one of the great advances in medicine. Before their discovery in 1928 and first use in the 1940, many people died of infections that are now preventable.
When used properly, antibiotics can save lives. However, people often forget that antibiotics only work for bacterial infections. Antibiotics either stop bacteria from reproducing or kill them.
So if your sore throat is caused by a virus, taking antibiotics will not do you any good. It turns out that their misuse is one of the greatest threats to healthcare worldwide, as it is leading to the emergence of antibiotic-resistant bacteria.
“Antibiotic resistance is mostly caused by unwise use [of antibiotics], including using them to fight diseases that are caused by viruses,” said Nurul Itqiyah Hariadi from Atmajaya University’s Medical School.
Resistance is what happens when bacteria adapt to antibiotics, using mechanisms to become immune to the drug. These resistant bacteria then survive.
“In nature, there will always be a small number of bacteria that have resistance. In a normal situation, these resistant bacteria are only small in number because they cannot compete with other bacteria that have no resistance,” Nurul said.
The more antibiotics we use, the more we generate resistant bacteria and therefore provide a definitive advantage for these bacteria in overcoming antibiotics.
The antibiotics become less effective the more we use them and eventually have no effect at all. These types of bacteria are called superbugs, which are resistant to certain types of antibiotics.
“Unwise use of antibiotics will kill bacteria that have no resistance. Therefore, the only bacteria that can survive and replicate themselves are resistant bacteria. These bacteria are becoming dominant,” said Nurul.
The speed at which bacteria develop resistance against antibiotics is also unmatched by medical advancement.
“A bacteria can become resistant toward antibiotics within one to two years of a certain antibiotic being invented. Meanwhile, the development of a new antibiotic could take from 10 to 15 years,” Nurul said.
Drug resistant infections are already on the rise with numbers suggesting that up to 50,000 lives are lost each year due to antibiotic-resistant infections in Europe and the US alone.
Globally, at least 700,000 die each year of drug resistance due to illnesses such as bacterial infections, malaria, HIV/AIDS or tuberculosis.

And things are looking to get worse. A study commissioned by the UK government suggests that resistance to antibiotics could lead to 10 million deaths per year by 2050 and cost US$100 trillion a year to combat.
Described as a looming global crisis, resistance affects all countries, including Indonesia, where more than 50 percent of antibiotic prescriptions are unnecessary as doctors often worry that patients may have bacterial infections.
Furthermore, people still think of antibiotics as the ultimate cure for all diseases. As many as 40 percent of adults in Yogyakarta City think that antibiotics can cure all diseases, with 71 percent of them believing that the drugs are needed to cure infections caused by viruses, according to a 2010 research paper published in the medical journal Antimicrobial Resistance and Infection Control.
Worried parents are also quick to give antibiotics to their children, with 30 percent of them giving their children the medicines for common colds and fever, according to a 2010 research paper by the Indonesian Caring Parents Foundation (YOP).
Research carried out by the Health Ministry in 2013 showed that 86.1 percent of people kept antibiotics at home without any prescription, meaning that they got them from drug stores.
This unrestrained use of antibiotics has created superbugs. One of the most dangerous is called NDM-1, which makes bacteria resistant to even some of the strongest antibiotics, including carbapenems.
Carbapenems are the most powerful antibiotics used as a last resort for many bacterial infections, such as E. coli.
“Even the most powerful antibiotics, carbapenems, no longer work. This superbug has appeared in Indonesia but we don’t know the prevalence,” Harry Parathon, head of the Antimicrobial Resistance Control Committee (KPRA), said.
According to research conducted at Cipto Mangunkusumo General Hospital in 2011, the superbug had been found in the hospital’s intensive care unit.
Another superbug found in Indonesia is Extended-spectrum -lactamases (ESBLs), which are bacteria that produce the enzyme beta-lactamase, which has the ability to break down commonly used antibiotics, such as penicillins and cephalosporins and render them ineffective for treatment.
If ESBL-producing bacteria cause an infection, a different antibiotic may be needed to treat the infection. Infections due to ESBL range from uncomplicated urinary tract infections to life-threatening sepsis.
superbug was found in 71 percent of E. coli in Indonesia, higher than the Asia Pacific average rate of 48 percent, according to a study published in the Antimicrobial Agents and Chemotherapy medical journal in 2011.
It was also discovered in 64 percent of Klebsiella, a bacteria that can cause different types of healthcare-associated infections, including pneumonia, bloodstream infections, wound or surgical site infections, and meningitis.
This emergence of superbugs has made it more difficult than ever to treat bacterial infections.
“The numbers for pneumonia, urinary tract infections and sepsis are increasing in Indonesia. Here, the death rate for sepsis has reached 76 percent, compared to around 40 percent in Europe,” Harry said.
Sepsis is a life-threatening condition that occurs when the immune system damages tissues and organs while fighting an infection. The reaction causes widespread inflammation, leaky blood vessels and abnormal blood clotting. The results can be organ damage and, in severe cases, blood pressure drops, multiple organ failures and death from septic shock.
A study conducted in a hospital in Bandung, West Java, in 2012, found that sepsis patients who received appropriate doses of antibiotics had lower mortality than those who did not.
“The early administration of appropriate antibiotic therapy for serious infection is associated with lower mortality, shorter duration of hospitalization, and lower health care cost,” the study said.
The study also found that more than half of the 47 antibiotics used by patients showed resistance rates of more than 50 percent.