Popular Reads
Top Results
Can't find what you're looking for?
View all search resultsPopular Reads
Top Results
Can't find what you're looking for?
View all search resultsCOVID-19 causes major setbacks for RI as TB high burden country
In many countries, human, financial and other resources have been reallocated from TB to the COVID-19 response.
Change text size
Gift Premium Articles
to Anyone
T
he theme “Clock is Ticking” of this year’s World Tuberculosis (TB) Day, which fell on March 24, rings so true to the world’s three TB high-burden countries – China, India, Indonesia and the other 48 TB burden countries.
The impact of COVID-19 on the TB response is going to be felt for a long time to come. TB diagnosis and treatment in high-burden countries dropped dramatically in 2020, reversing years of progress.
Prior to the COVID-19 pandemic, many countries were making steady progress in tackling TB, with a 9 percent reduction in incidence seen between 2015 and 2019 and a 14 percent drop in deaths in the same period. High-level political commitments at global and national levels were delivering results.
However, a new report from the World Health Organization shows that access to TB services remains a challenge, and that global targets for prevention and treatment will likely be missed without urgent action and investments.
Approximately 1.4 million people died from TB-related illnesses in 2019. Of the estimated 10 million people who developed TB that year, some 3 million were not diagnosed with the disease, or were not officially reported to national authorities.
The situation is even more acute for people with drug-resistant TB. About 465 000 people were newly diagnosed with drug-resistant TB in 2019 and, of these, less than 40 percent were able to access treatment. There has also been limited progress in scaling up access to treatment to prevent TB.
Some of this was due to a repurposing of GeneXpert machines, which are typically used to diagnose TB, for COVID-19 testing and some due to enforced lockdowns restricting access to TB treatment and services.
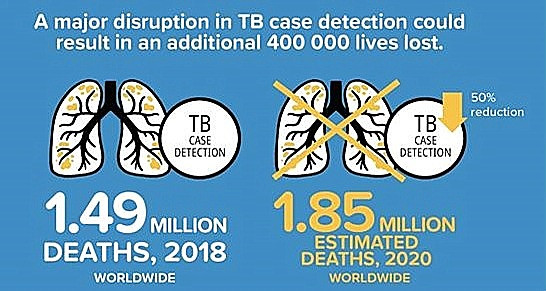
Experts estimate as many as 400,000 additional TB deaths may have occurred in 2020 and some of those will also include TB health care workers who were redeployed to the COVID-19 front lines.
Disruptions in services caused by the COVID-19 pandemic have led to further setbacks. In many countries, human, financial and other resources have been reallocated from TB to the COVID-19 response. Data collection and reporting systems have also been negatively impacted.
According WHO report, data collated from over 200 countries has shown significant reductions in TB case notifications, with 25-30 percent drops reported in 3 high burden countries – India, Indonesia, the Philippines – between January and June 2020 compared to the same six-month period in 2019. These reductions in case notifications could lead to a dramatic increase in additional TB deaths, according to WHO modelling.
In 2020, COVID-19 surpassed TB as the world’s top infectious killer but as we transition to COVID-19 recovery, we can, unfortunately, expect to a return to even higher rates of TB infection and mortality in countries that already experienced a high burden.
The statistics are alarming. The Stop TB partnership last year estimated that COVID-19 would produce an additional 6.3 million cases of TB between 2020 and 2025. Last week it revised those figures, and the new scenario is worse than we thought—12 months of COVID-19 has reversed 12 years of progress on TB.
COVID-19 must serve as an inflection point: We need to apply some of the lessons learned from COVID-19 to all future infectious disease control The countries who have led the best responses to the pandemic have followed the science, but science alone won´t be enough. As the pandemic has shown, political will and commitment is vital too.
The Stop TB Partnership is right when it says that the world needs to strategically prepare for future airborne pandemics building on the investments and strategies that have been part of the TB response. The tools and strategies that we have employed in responding to the current pandemic—trace, test, isolate—are ones we´ve been implementing successfully for decades and decades with TB.
We have the tools to tackle TB, we need decision-makers to act fast.
While most countries are gearing up to roll out COVID-19 vaccines for their citizens. The year 2021 marks the 100th year of the first ever TB vaccine—BCG.
We do have the BCG vaccine for TB, discovered 100 years ago, but it doesn’t prevent respiratory disease, which is the most common form of TB in adults. It is 70 percent to 80 percent effective against the most severe forms of TB, such as TB meningitis, in children. We´ve long needed a new and better vaccine for TB—100 years is an outrageously long time.
COVID-19 has demonstrated just how interconnected we all are. No one is safe until we are all safe. My hope is that global interventions such as COVAX, working for global equitable access to COVID-19 vaccines, might provide the template for how we think about disease control, including vaccination, going forward. It clearly must be based on the moral imperative of equity and driven by scientific reasoning—acknowledging that a failure to vaccinate or eliminate diseases in one country will have a knock-on effect everywhere else. We can and must apply the same approach to ending TB.
There´s a lesson here for the TB world. Unlike COVID-19, we do have treatments that can both prevent, treat and cure TB for most people. We need to up the ante when it comes to tracing and testing. COVID-19 has shown how important it is to slow down a global pandemic. We can slow down TB too.
We’ve seen how fast the Access to COVID-19 Tools (ACT) Accelerator—set up by the WHO and partners—has facilitated the manufacture and delivery of 120 million high-quality rapid antigen diagnostic tests to countries that lack the laboratory facilities or trained health workers to implement PCR tests. As many as 500 million tests are planned for distribution before October 2021. This feat was accomplished in months; by contrast, it took five years for a similar facility to produce the first WHO-approved rapid diagnostic test for HIV.
ACT’s vaccines pillar— also known as COVAX—is working for global equitable access to COVID vaccines, shining a light on the inequity of vaccine access between rich and poor countries thus far 30 million vaccine doses have finally been distributed to low- and middle- income countries—compared to the 100 million and counting in the United States alone—but it is clearly insufficient.
Both these initiatives are exciting because they embody the ideas of equity and evidence-based science, and recognize just how interconnected we all are. The vaccine debate of late has not just been about the right of all people to access a vaccine regardless of where they are born. It has been just as much about the scientific need to do so: a failure to vaccinate or eliminate disease in one country will have an effect everywhere else.
The same is true for TB: TB anywhere is TB everywhere. In this interconnected world, none of us are safe until all of us are safe. Out of crises, new opportunities can arise. We`re at a defining moment in infectious disease control. We need to seize the moment and take real action.
***
The writer is the president and CEO of the New York-based global health organization Vital Strategies, working, among others, on tobacco control and partnership for healthy cities across the world including in Indonesia.