Popular Reads
Top Results
Can't find what you're looking for?
View all search resultsPopular Reads
Top Results
Can't find what you're looking for?
View all search resultsBalancing scales: Crafting a sustainable healthcare future
Healthcare providers are the primary touchpoint for patients. Their actions are therefore critical to ensuring cost management while delivering positive outcomes.
Change text size
Gift Premium Articles
to Anyone
T
he pandemic, while a distant memory for many of us, has left a lasting impact on healthcare systems worldwide, including in Indonesia. Driven by pent-up demand and increased health awareness, Indonesian healthcare spending has surged, with medical inflation reaching double digits and health insurance claims increasing by nearly 25 percent in 2024, outpacing the Asian average.
A multitude of factors are driving this change — increase in input costs for drugs and consumables, exchange rate deterioration, greater awareness among patients, greater utilization of health resources and the ever-present fraud and abuse that plagues the industry.
These dynamics are making the economics unviable for participants across the healthcare ecosystem. As a result, several healthcare providers have had to respond by transferring elevated costs to patients and payers. Health payers are exploring avenues to refine claims process and improve the cost-effectiveness of treatments. Patients are having to postpone elective medical treatment or seek care at alternative locations.
Solutions need to be found and will require stakeholders to work collaboratively to ensure the best interests of the patient and the nation are served, while ensuring individual motivations are not adversely impacted.
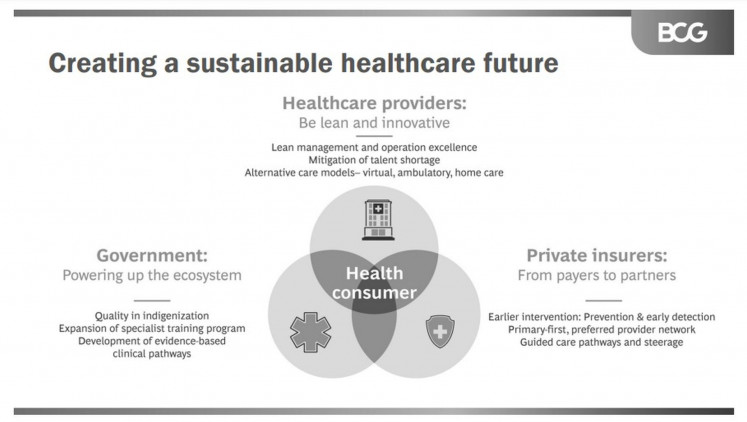
Healthcare providers: Be lean yet innovative
Healthcare providers are the primary touchpoint for patients. Their actions are therefore critical to ensuring cost management while delivering positive outcomes.
There are three dimensions which providers need to look at. First, there is a need to apply the classic principles of lean day-to-day management of healthcare facilities — procurement excellence to maximize value in purchase of drugs and consumables, lean service operations to maximize clinician utilization and redesign of care delivery processes to improve throughput. Clinicians are the costliest and the scarcest resource in a hospital setting and driving their utilization and productivity is critical for optimal business economics.
Second, the Omnibus Health Law now provides private providers with the opportunity to deploy foreign medical talent. It is imperative that providers plan well and leverage this opportunity to mitigate crucial clinical talent challenges. Providers could proactively partner with international medical groups of repute to bring the much-needed talent, upskill local Indonesian talent and get access to clinical protocols to enable care delivery at cost.
Third, there is a need to embrace alternative models of care — virtual, telehealth and ambulatory care. In most developed healthcare systems, alternative care models are gradually becoming the norm, rather than the exception, be it virtual wards in the United Kingdom’s NHS, or ambulatory surgical centres being piloted by several private providers in the region. With these models, providers have the opportunity to not just reduce cost, but also enhance patient experience.
Health insurers: From payers to partners
Health insurers have traditionally been payers of care delivery. It is time for them to pivot from being mere “wallets” to becoming “activist partners” managing the health for their policyholders. They can do so by three key interventions.
First and foremost, insurers need to intervene earlier in patient journeys through wellness, prevention and early detection programs. Early treatment costs are two to four times lower than late-stage treatments. Several insurers in ASEAN have taken steps in this direction, for example, incentivizing gym memberships and healthy food habits, or offering preventive health management services. In Singapore, with the advent of Healthier SG, the state itself has been leading the push.
Second, insurers need to establish primary-care-first, preferred healthcare provider networks. A primary-care-first network, in which general practitioners (GPs) and primary care providers act as the first point of contact, can help minimize the need for expensive tertiary care. This needs to be coupled with creating preferred partnerships and hybrid delivery models enabling care in lower acuity settings. Insurers could also incentivize treatment in lower-acuity settings, such as shifting from inpatient to day surgery, or from hospitals to community clinics.
Third, insurers need to take control over the patient journey. Patients often lack adequate information to judge which care option is most appropriate. The choice of care then gets influenced by intermediaries, friends and family, or online reviews. Insurers have access to extensive data regarding clinical outcomes and care cost at individual providers, and are in a good position to guide their patients regarding choice of treatment and treatment provider. Hence, it is important that insurers implement interventions to proactively guide patients and steer them toward the most appropriate provider and care pathway.
The state: Powering up the ecosystem
The role of the state is equally essential. Important first steps have been taken regarding localization of medical devices and allowing foreign clinical talent to practice. A lot more can be done.
First, there has been a commendable push toward indigenization. There is now a need to ensure locally manufactured drugs, consumables and devices are of excellent quality, which will give clinicians the confidence to use local products. Besides reducing costs, a “quality indigenous” product will also build self-reliance and shock-proof the local healthcare industry from supply chain and exchange rate fluctuations.
Second, there is a need for continued investment in the local clinician talent pool by expanding specialist training programs. While access to foreign doctors is an important immediate measure, building the pipeline for local specialists is equally essential to ensure a stronger future for Indonesia.
Third, there is an opportunity to develop or bring in evidence-based clinical pathways with buy-in of local clinicians. This will not only drive improvements in quality of care, it will also help standardize and control costs. Several health systems in the United States, including Geisinger Health System's ProvenCare and Intermountain Healthcare's Heart Failure program, have shown significant benefits using this approach. Indonesia can benefit from adopting similar practices.
Shared steps for success
In many developed health systems, an inherent integration of payers and providers, alongside funding limits, serves as a natural force for the above actions. In Indonesia, however, payers, providers and individuals will need to drive concerted efforts to adapt their roles and practices. It is time for healthcare players to take a shared step toward success. Only through collaboration can Indonesia’s healthcare industry achieve a more sustainable future for all.
***
Anurag Agrawal is a managing director and partner at Boston Consulting Group, where Yishu Pi is a project leader. The authors acknowledge Boston Consulting Group’s principal Alan Ong, knowledge expert Ayano Uehara and project leader Boon Kiat Lee for contributing their insights to this article.