Popular Reads
Top Results
Can't find what you're looking for?
View all search resultsPopular Reads
Top Results
Can't find what you're looking for?
View all search resultsUS confirms first bird flu case without animal contact
The person who tested positive for bird flu was the 14th to do so in the United States this year, and the first without known contact with animals.
Change text size
Gift Premium Articles
to Anyone
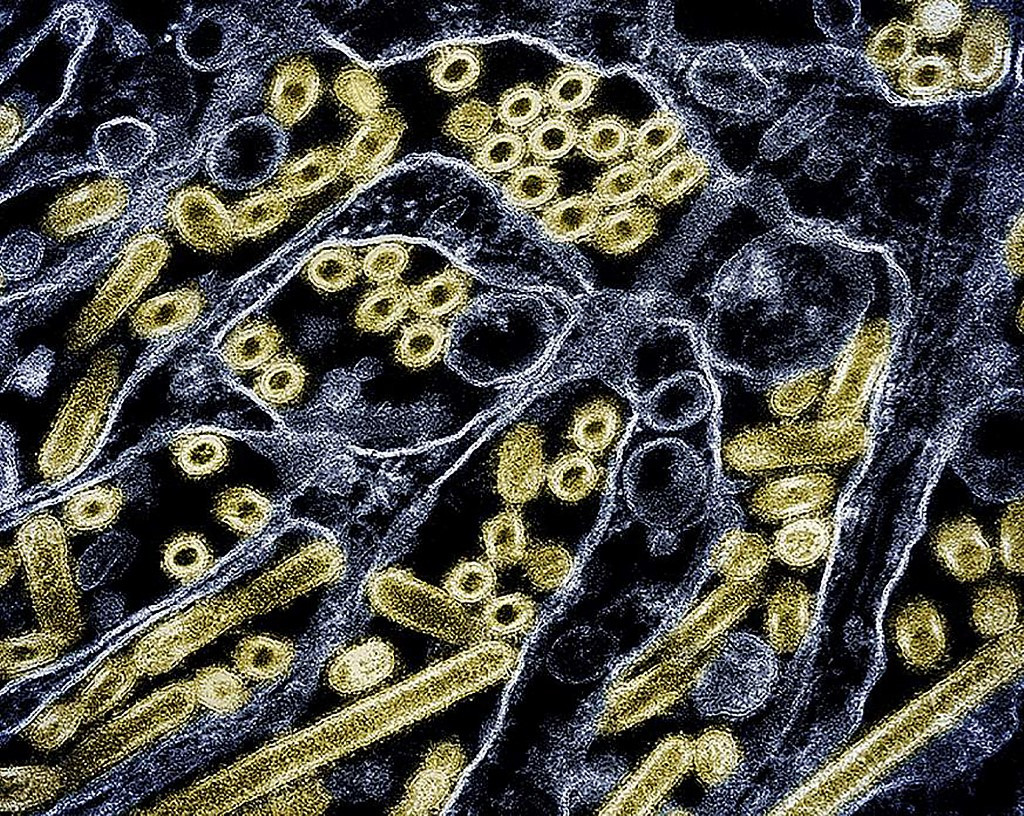 This handout picture courtesy of CDC and NIAID released on May 24, 2024 shows a colorized transmission electron micrograph of avian influenza A H5N1 virus particles (gold), grown in Madin-Darby Canine Kidney (MDCK) epithelial cells. Mice fed raw milk infected with bird flu experienced high levels of virus in their lungs, according to a study published May 24, 2024 that underscores the danger to humans of consuming the drink.
Over the past few years, a highly pathogenic avian influenza virus called HPAI H5N1 has spread to infect more than 50 animal species, including dairy cattle in the United States from March. (AFP/CDC and NIAID)
This handout picture courtesy of CDC and NIAID released on May 24, 2024 shows a colorized transmission electron micrograph of avian influenza A H5N1 virus particles (gold), grown in Madin-Darby Canine Kidney (MDCK) epithelial cells. Mice fed raw milk infected with bird flu experienced high levels of virus in their lungs, according to a study published May 24, 2024 that underscores the danger to humans of consuming the drink.
Over the past few years, a highly pathogenic avian influenza virus called HPAI H5N1 has spread to infect more than 50 animal species, including dairy cattle in the United States from March. (AFP/CDC and NIAID)
A
person in the state of Missouri has become the first in the United States to test positive for bird flu without a known exposure to infected animals, authorities said on Friday.
The adult patient, who has underlying conditions, was admitted to hospital on Aug. 22, received antiviral medications against influenza, then recovered and was discharged, according to statements from the Centers for Control and Disease Prevention (CDC) and the Missouri Department of Health and Senior Services.
As the patient's flu type appeared suspicious on an initial test, it was sent for additional testing in state and federal laboratories, which revealed it was H5, also known as avian flu or bird flu.
The CDC said it had not identified any transmission to the patient's close contacts or any other person.
Scientists have voiced concern about the growing number of mammals becoming infected by bird flu, even if cases in humans remain rare.
They fear a high rate of transmission could facilitate a mutation of the virus, which could enable it to be passed from one human to another.
Contacted by AFP, the World Health Organization said on Saturday it was "encouraging that the national disease surveillance system has identified this case, that the patient received antiviral treatment, and that no further cases have been detected among close contacts".
"It is critical that investigations into the patient's exposure are continued, as indicated by national and state authorities, to inform further prevention and response activities," said Dr Maria Van Kerkhove, the WHO's director of epidemic and pandemic preparedness and prevention.
"WHO strongly supports US efforts for surveillance of zoonotic influenza across human, environmental and animal sectors," Van Kerkhove continued.
"It is important to understand the circulation of avian influenza in poultry, wild birds and other animals in the state," she said of Missouri.
"Stronger disease surveillance in animals is essential to protect animal and human health."
No animal contact
The person who tested positive for bird flu was the 14th to do so in the US this year, and the first without known contact with animals.
Indeed, "no H5 infection in dairy cattle has been reported in Missouri," said the Missouri health department, though "some H5 cases in commercial or backyard flocks and wild birds have been reported."
All previous bird flu cases in the United States have been among farmworkers, including the very first, in 2022.
Bird flu is most commonly found in wild birds and poultry, but has more recently been detected in mammals, with an outbreak in cattle seen across the country this year.
It can occasionally infect humans through close contact or contaminated environments.
While the CDC continues to assess the risk to the public as low, "circumstances may change quickly as more information is learned", it said.
In the decades since H5 has been found in humans, there have been rare cases where an animal source cannot be identified.
But there has so far not been evidence of sustained human-to-human transmission, which would significantly increase the threat level.