Popular Reads
Top Results
Can't find what you're looking for?
View all search resultsPopular Reads
Top Results
Can't find what you're looking for?
View all search resultsLiving with autoimmune disease during COVID-19 pandemic
Indonesians with autoimmune diseases face their own set of pandemic challenges
Change text size
Gift Premium Articles
to Anyone
“I’ve never heard of people with autoimmune diseases being infected by the coronavirus. Are we perhaps immune to it?” David (not his real name) wrote in a private autoimmune Facebook group.
In another autoimmune group, Yakub (not his real name) wrote a similar message.
“Is it true that people with Lupus produce antibodies that can kill the coronavirus?”
Such misconceptions can be deadly during the pandemic. And yet, they exist because there is a lack of understanding about autoimmune diseases, as well as the coronavirus.
There are more than 80 types of autoimmune diseases in the world. Each of them still a mystery in the medical world, as their exact causes are unknown and their medications can only keep symptoms at bay. A lot of medical practitioners, as well as patients, are still grappling to understand and manage these chronic diseases, in which the body’s immune system attacks its own organs. And their struggles amplified when the COVID-19 pandemic struck.
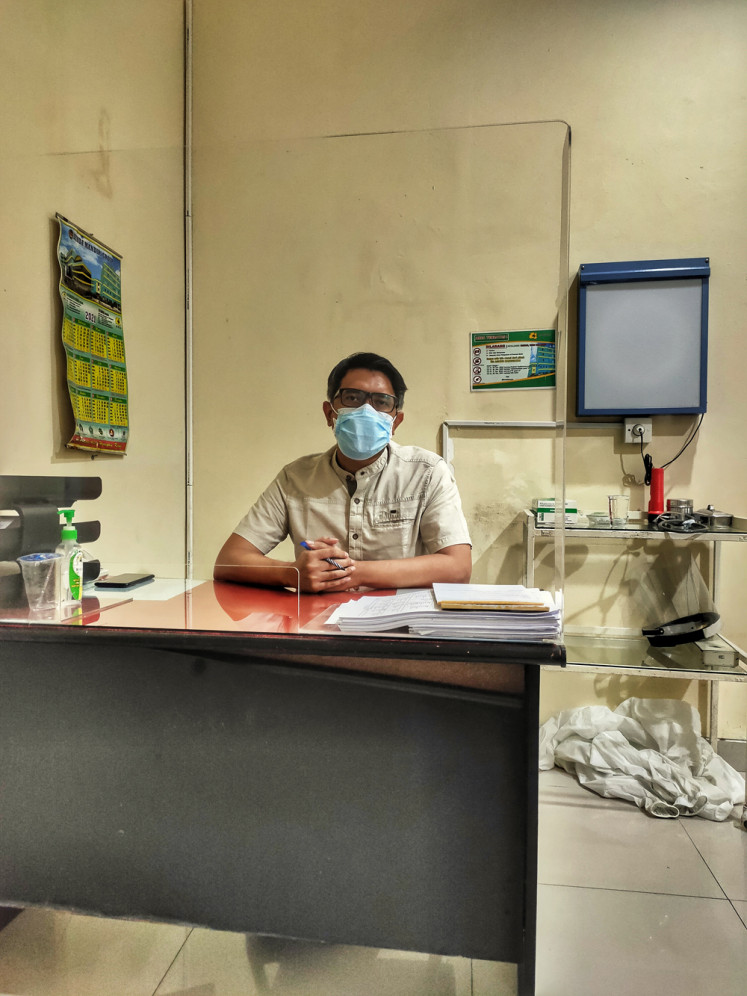
“Autoimmune diseases are a disregulation of the immune system,” Dr. Fadrian, internist at Agung Hospital, Central Jakarta, said during an interview with The Jakarta Post at the hospital on July 6. “It doesn’t mean that you have a specific antibody against COVID-19.”
In fact, autoimmune diseases are considered a comorbidity that increases the risk of patients getting infected by the coronavirus.
“And when they do, their condition usually gets worse very quickly,” the internist added.
Simultaneous attack
On Nov. 12, Dessy Mardiana, a 43-year-old entrepreneur in Yogyakarta, tested positive for COVID-19 and was admitted to the hospital. At that time, she had mild flu-like symptoms and a fever. Dessy has systemic lupus erythemathosus (SLE) and was experiencing difficulty breathing, with an oxygen saturation level between 88-92.
The next day, her condition got a lot worse and she had to be admitted to an intensive care unit (ICU).
Nothing specific: Dr. Fadrian, an internist at Agung Hospital, Central Jakarta, said having an autoimmune disease did not mean someone had a specific antibody against COVID-19. (JP/Sylviana Hamdani)“My albumin, kidney function and hemoglobin dropped at the same time,” she said during a phone interview on July 14. “In the meanwhile, my blood sugar soared like never before.”
Dessy also experienced blood coagulation and became paralyzed.
“As a Lupus patient, I’m used to getting hospitalized,” the mother of five said. “But it was very different. COVID-19 attacked many different parts of my body at the same time. My medical treatment was a race against time.”
Luckily, Dessy's illness was detected early. She was admitted to the hospital as soon as her diagnosis was confirmed. After 23 days of being hospitalized, Dessy beat the coronavirus and returned home.
Get tested
“Never underestimate flu-like symptoms during the pandemic, especially when they’re accompanied by a fever above 37.5 degrees Celcius,” Dr. Fadrian said.
The internist suggested people with autoimmune diseases get a PCR test when they have flu-like symptoms and a high fever.
They should also get a PCR test when they have come into close contact with anyone confirmed to have contracted COVID-19.
“You should get tested if you’ve been within 1.8 meters of someone who tests positive for COVID-19, if you eat or share utensils with them or are exposed to their cough or sneeze,” Dr. Sandra Sinthya Langow, a rheumatologist at Siloam Hospital Lippo Village said during an Instagram live session on the @autoimmunewarrior.id account on July 4.
Long COVID-19
People with autoimmune diseases are also susceptible to long COVID syndrome, in which symptoms of the disease continue long after the patient has been cleared of the coronavirus.
Basri, a 33-year-old teacher in Bandung, West Java, was happy when he was discharged from the hospital seven days after he tested positive for COVID-19. But his happiness was short-lived.
“Two weeks after being discharged from the hospital, I’m still experiencing terrible headaches, stomach aches and nausea,” the man living with rheumatoid arthritis said during a phone interview on July 18. “I couldn’t do any work at all.”
Basri consulted his doctor, who then confirmed that he had a case of long COVID.
Online answers: Indonesians with autoimmune diseases face their own set of pandemic challenges and often go online to find answers. (JP/Sylviana Hamdani)“Approximately 80 percent of COVID-19 patients will experience long COVID symptoms, which include malaise, joint and muscle pains, headaches, stomach aches, nausea and coughing,” Dr. Sandra said. “Some even develop lung problems after COVID-19.“
These symptoms may persist for between three to 12 months after the patient has tested negative for the coronavirus.
In facing long COVID, the rheumatologist advises patients to take more rest and get better nutrition. They should immediately see their doctor if their condition worsens or they experience difficulty in breathing.
Second COVID-19 infection
Dessy became wary when more and more of her neighbors became infected with COVID-19 in early June.
“Our house became besieged with those infected,” she said.
A week later, Dessy, her husband and their five sons developed flu-like symptoms all at once. A PCR test confirmed that all of them had been infected by the coronavirus.
“I was so shocked I had gotten infected by the coronavirus for the second time,” she exclaimed.
Luckily, their symptoms were mild and they were allowed to self-isolate at home.
“When you’ve been infected by the coronavirus, your body will develop an antibody for the virus,” Dr. Fadrian said. “But the main problem is the virus mutates very quickly. Therefore, it is possible that we get infected by a newer variant.”
The only way to avoid getting infected by the coronavirus multiple times, according to the doctor, is to maintain health protocols and get vaccinated.
Vaccination for the autoimmune
Getting vaccinated is not a simple matter for people living with autoimmune diseases. First of all, they have to be examined by their doctor and deemed to be in a stable condition to receive the COVID-19 vaccination.
“To be allowed the COVID-19 vaccination, people with lupus should have a normal level of Anti-ds DNA [determined by a laboratory test] and no longer experience mild fevers, muscle or joint pains,” Dr. Fadrian said.
When your doctor approves the vaccination, he or she will issue a letter that states your condition is stable and you are eligible for the vaccination. You should then show the letter to the medical practitioners at the vaccination center.
“If the patient doesn’t have a history of blood coagulation or stroke, any COVID-19 vaccine will be fine,” the internist said. “If not, they should then choose any vaccine other than AstraZeneca.”
Will people with autoimmune diseases fall ill after the vaccination?
“No more so than any of us,” Dr. Sandra Sinthya Langow said. “Having a mild fever or nausea for three to five days after getting vaccinated is normal. We have to remember that the benefits [of getting vaccinated] are much, much greater than the inconveniences.”
'Prokes' lifestyle
In order to protect themselves against the coronavirus, Dr. Fadrian advises people living with autoimmune diseases to always observe the same "prokes" (health protocols) as anyone else.
“Immunity-boosting supplements might do more harm than good to people with autoimmune diseases,” Dr. Sandra said. “You can actually get all the necessary nutrients by consuming fresh fruits and vegetables.”
For people with SLE that have photosensitivity and cannot get any sun exposure, they may take vitamin D supplements. Their doctor will determine the correct dosage to maintain their condition.
Despite the pandemic, people with autoimmune diseases should see their doctor regularly to monitor their condition.
“It is proven that people with autoimmune diseases that have their condition under control are less susceptible to the coronavirus,” Dr. Sandra said. “You can use telemedicine facilities if you’re afraid of going to the clinic or hospital during the pandemic.”