Popular Reads
Top Results
Can't find what you're looking for?
View all search resultsPopular Reads
Top Results
Can't find what you're looking for?
View all search resultsEqual access to funding, Big Pharma commitments essential in global COVID-19 resilience
The Jakarta Post spoke with Health Minister Budi Gunadi Sadikin about strategies to lessen the impact of the COVID-19 third wave, the country’s health system and how Indonesia’s G20 presidency will improve global resilience against the virus.
Change text size
Gift Premium Articles
to Anyone

For almost two years, the COVID-19 pandemic has battered the world and severely tested Indonesia’s healthcare system. Now, Indonesia is facing yet another wave of infections, triggered by the highly contagious Omicron variant.
The Jakarta Post's Nina A. Loasana, Marchio Irfan Gorbiano and Adisti Sukma Sawitri spoke with Health Minister Budi Gunadi Sadikin about strategies to lessen the impact of the COVID-19 third wave, the country’s health system and how Indonesia’s G20 presidency will improve global resilience against the virus. The following is an excerpt from the interview.
Question: People and businesses have returned to high mobility and normal activities despite the pandemic not being over. Now that Omicron is on the rise, what are the ministry’s strategies to minimize hospitalizations and prevent deaths during the peak of Omicron spread?
Answer: We rely on four strategies: enforcement of health protocols or the 3M [mask wearing, frequent handwashing and maintaining physical distance], strengthening surveillance or the 3T [testing, tracing and treatment], accelerating vaccination and providing therapeutics. The first three strategies are upstream responses targeted at healthy individuals while therapeutics is our downstream response.
We need to focus on our upstream strategies [to effectively mitigate another wave of transmission]. Enforcement of health protocols, especially wearing a mask, is crucial. We also need to carry out vigorous testing. The World Health Organization [WHO] requires us to test one person in every 1,000 per week, [which in Indonesia's case is] around 270,000 people per week or 48,000 people per day. Our testing rate is quite good at the moment, around 200,000 people a day, far above the WHO minimum testing benchmark.
However, at the moment we need to improve public discipline to self-isolate or to go to isolation centers if they test positive for COVID-19.
If you contract COVID-19, don't panic, isolate yourself at home immediately. Take vitamin C and vitamin D supplements, implement a healthy lifestyle, and you'll recover soon Insya Allah [God willing]. Don't panic and rush to the hospital. Let the hospital treat only moderate and severe cases.
During the second wave of infections last year, people died in self-isolation because they could not access emergency care, how will the government prevent similar incidents from happening?
The second and the third wave of infections are very different from each other. During the second wave, the hospitalization rate was high but during the third wave it is quite low. Due to the stark difference between the characteristics of the second and the third wave, we’ve decided to shift our focus from hospital treatment to at-home treatment and the use of telemedicine.
We admit that telemedicine services are not available in all cities in Indonesia and can only be accessed in big cities. But we're working together with public health centers [Puskesmas], state-owned hospitals and regional hospitals, to provide online health consultation services for COVID-19 patients across the country. We'll also ensure that all healthcare facilities have sufficient medicine supply for patients.
I want to emphasize once again that the characteristics of the second and third waves are very different. As the hospitalization rate was high during the second wave, many COVID-19 patients died because they couldn’t access medical services. However, during the third wave there will be a lot of COVID-19 patients who won’t need hospital care.
The government has imported COVID-19 medicines molnupiravir and Paxlovid. Are they already available at drugstores?
Based on the advice from five medical professional associations, the Health Ministry has recommended three antiviral drugs for COVID-19 namely favipiravir, molnupiravir and Paxlovid.
We have more than 20 million tablets of favipiravir at the moment. The ministry has procured 400,000 tablets of molnupiravir and has distributed them to regional health facilities. It is also on the process of distributing 400,000 tablets of molnupiravir to pharmacies across the countries. The drugs would cost round Rp 500,000 [US$34.80] to Rp 600,000 per regime of 40-80 tablets.
But I need to emphasize that these drugs can only be purchased with a prescription. We don't want people to hoard the drugs in their homes. Drugs should be kept at pharmacies to effectively maintain their efficacy. If people buy the drugs for personal stocks and they don't contract COVID-19, the drugs will expire and go to waste. If the drugs remain at pharmacies, they can be distributed to people who really need them.
We're also in the process of importing Paxlovid and we hope that by early February the drugs will arrive in the country.
The government has decided to give half doses of the Pfizer and Moderna vaccines as booster shots. A study from Yale University found that even a full dose of the Pfizer vaccine was not effective to protect against Omicron. Have there been results on the effectiveness of both vaccines in Indonesia?
I've read the Yale University research and found out that it actually involved a very small cohort of around 110 subjects, we have bigger samples in our research on booster doses.
The Yale study suggested that one dose of the Pfizer vaccine can't protect against Omicron, but I have to clarify that there are currently no vaccines that can protect people against Omicron. It's not something new, even if we are vaccinated five times, we can still catch an infection.
The main goal of vaccination is not to prevent transmission but to train our antibodies to recognize, fight and beat the coronavirus.
So far, no scientific study has determined the level of antibodies needed to protect someone against COVID-19, but doctors require a minimum antibody titer of 250 for convalescent plasma treatment.
Our research study suggested that one dose and a half dose of the Pfizer booster shot could increase antibody levels from 100 to 7,000-8,000. However, the difference between a half dose and one dose of the booster vaccine is miniscule. For example, a half dose of the Pfizer vaccine could improve the recipients’ antibody titer to 7,900 and one dose of the Pfizer booster shot could improve antibody titer to 8,100. Although one dose of the vaccine could induce a higher antibody response than a half dose, the difference is not significant, as both could induce antibody levels far above the 250 threshold.
The government has just started COVID-19 vaccination for children and the nationwide booster rollout. Will the government increase vaccine imports this year, and from which producers?
The government has enough vaccine supply for adult primary vaccination and booster shot rollout. Most of our vaccine supplies came from donations and this year we’ll also receive a lot of vaccine grants. The only vaccine that we will purchase this year is the Sinovac vaccine for children.
So far, there are only three vaccines for children aged 5-11 that have been approved [by the WHO], namely Pfizer, Sinopharm and Sinovac. Children’s bodies are fragile so we chose the vaccine brand with the least adverse events following immunization, which is Sinovac.
How will the government speed up vaccination in remote areas that still have low vaccination coverage such as Papua?
So far, we have rolled out 183 million doses of COVID-19 vaccines. Almost 70 percent of the targeted population have received the first dose and almost 50 percent have been fully vaccinated. We have achieved the WHO's target of fully vaccinating 40 percent of the population in December and we may achieve the WHO's next target of fully vaccinating 70 percent of the population by June, earlier in March.
We do have a vaccine disparity issue in Papua, which is mostly caused by social issues. Papua residents need to be constantly reminded that vaccination is important to protect ourselves and our families from the coronavirus.
We have carried out various programs to boost vaccination in remote areas, including giving motorcycles and buffalos as door prizes for vaccine recipients, working together with tribal leaders, church leaders and mosque leaders. Our programs have shown positive results in some regions such as Aceh and West Sumatra but we admit that it's hard to accelerate vaccination in Papua. They need more education on the importance of vaccination.
Building global health architecture has been one of the major themes of Indonesia’s G20 presidency. President Joko “Jokowi” Widodo has vowed to push the establishment of a global health fund to finance health emergencies, including the COVID-19 pandemic. What will be the key tasks that Indonesia plans to accomplish in its G20 leadership?
The main topic under the global health architecture is reforming global health system resilience. We have submitted three priority issues for the topic: building health system resilience, harmonizing global health standard protocols and redistributing manufacturing hubs and research hubs to developing countries to reach global health system resilience.
We expect five outputs related to building health system resilience, the first one is to create a global health fund of $15 billion per annum for 10 years so we can gather up to $150 billion. The IMF, for example, has $200 billion and the World Bank has $ 600 billion, so $150 billion is enough.
Second, we want commitment from big manufacturers and pharmaceutical-producing countries so that we can use the funds to access health emergency countermeasures if another global pandemic strikes. In the early days of the pandemic, we could not buy masks, ventilators or medicines despite having money. There should be a commitment to open access to emergency vaccines, diagnostic tools and medicines.
The third output is we want to integrate platforms for whole genome sequencing; our radar for viruses. So, if a new variant emerges in South Africa, then it is detected in Egypt, we can know immediately. The fourth output is we want to create a global health passport. At the moment, each country has different testing policies, quarantine periods and different travel requirements, we want to harmonize them all using technology. Just like passports that have one standard procedure across the world.
Lastly, we want to build a manufacturing and a research hub. If, let’s say, we have a zombie outbreak in the United States, and the US is annihilated, we could move the research to Israel, to Brazil or Indonesia. We believe that countries in Africa and Asia should have a research and manufacturing hub for emergency medical countermeasures.
Aside from pandemic control, the government is also considering eliminating service classes and premium tiers for the National Health Insurance (JKN) program. Do you support this plan?
At the Health Ministry, we want the Health Care and Social Security Agency [BPJS Kesehatan] to cover as many people as possible. It's better to cover 270 million people but with lower service classes than covering only 100 million people with higher service classes. There should be equity in accessing health care.
Now, the level of health services will depend on the state's capacity to provide universal health coverage for all citizens. Our economy is improving, so I hope the level of health service that we provide can increase as well. But the bottom line is that we want the same health services for all citizens.
Learning from the pandemic and the state of Indonesia’s health system, what will be your focus in improving health care for citizens?
Pak President gave me three tasks: COVID-19 vaccination, pandemic mitigation and reforming our healthcare system.
We've analyzed [all problems] and we'll reform six sectors. First, is the primary care service reform. We want to shift our focus to promotive measures instead of curative efforts. We want to create healthy people instead of treating sick people, because now most of our budget went to hospital treatment instead of promoting a healthy lifestyle.
We have launched many programs to achieve this goal, including adding primary immunization for children from 11 types of vaccines to 14, increasing antenatal care from four times to six times and requiring all pregnant women to have an ultrasound examination to reduce maternal and newborn deaths.
The second is reforming health service delivery. We don't want Indonesian citizens to seek medical treatment overseas because it means that we have poor healthcare quality.
Third, we want to reform the resilience of our healthcare system. Indonesia has a lot of natural disasters and epidemics. We want to secure the supply chain of medicines, medical devices and vaccines. We want to manufacture them in the country so we won’t rely too much on other countries. We want to ensure that we have enough healthcare workers as well. So that we have enough nurses and vaccinators if another pandemic occurs.
The fourth is we want to reform health financing and BPJS Kesehatan. The fifth one is reforming healthcare providers by increasing the number of doctors, improving their quality and ensuring equal distribution of health workers across the country.
The sixth goal is reforming healthcare technology including through information technology or biotechnology.
You have been on the job for about a year, which is quite different from your professional background as a banker. What do you think of the journey so far? And how does your previous professional experience help you with your current duties?
There are a lot of smart people in the Health Ministry so the only thing that I have to do is consolidate and direct them so that they can use their energy and time to achieve the same goals.
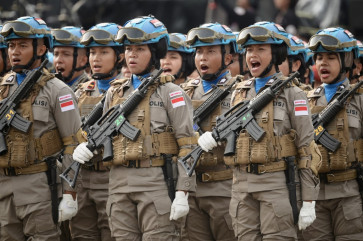
Our vaccination rollout is successful not only because of my own efforts. I believe police officers, soldiers, BIN officials and private companies work the hardest to roll out COVID-19 vaccines. Honestly, I was surprised at Indonesia’s social power. As long as we can explain the benefits of something and convince people that it’s a good thing to do, we can create a movement.
If the Health Ministry carries out the vaccine rollout by itself, it will not be successful. If we take an exclusive approach, it won’t work so we need to take an inclusive approach. The vaccination program is owned by the ministry but the movement is owned by everyone. So, I want to thank all Indonesian citizens and also thank Pak President for leading us in the fight against COVID-19.