Popular Reads
Top Results
Can't find what you're looking for?
View all search resultsPopular Reads
Top Results
Can't find what you're looking for?
View all search resultsInnovative reproductive health efforts, financing crucial during pandemic
Concerted efforts and innovative financing for sexual and reproductive health and rights in Asia and the Pacific are critical as the pandemic rages on.
Change text size
Gift Premium Articles
to Anyone
T
he Asia-Pacific region has witnessed very rapid developments over the past decades, with economic growth resulting in corresponding improvements to health services and infrastructure.
However, the benefits have not been enjoyed equally across populations, according to Ashish Bajracharya, the Population Council's deputy director for global country strategy and regional representative for South and East Asia.
He said that despite the economic growth, vast swathes of the population still had unmet needs in sexual reproductive health and rights (SRHR).
“In many countries, out of pocket expenditures continue to finance most healthcare expenditures, and these are unjustly reserved for the elite few in terms of quality as well as timeliness,” said Bajracharya.
He said he was aware that sociodemographic processes were at play, such as urbanization and labor migration, that exposed vulnerable populations to additional health risks.
“It is critical to work toward universal health coverage and to promote sustainable financing strategies, including heightening the commitment of state resources for SRHR to address some of these issues,” he said in his introductory remarks at the opening of the sixth session of the 10th Asia Pacific Conference on Sexual Reproductive Health and Rights (APCRASRH10), held virtually on Aug. 31.
The conference, which explored the theme "Innovative financing for sexual and reproductive health and rights in Asia and the Pacific", is part of a series organized by the APCRSHR10 steering committee, the United Nations Population Fund (UNFPA) and the Citizen News Service (CNS).
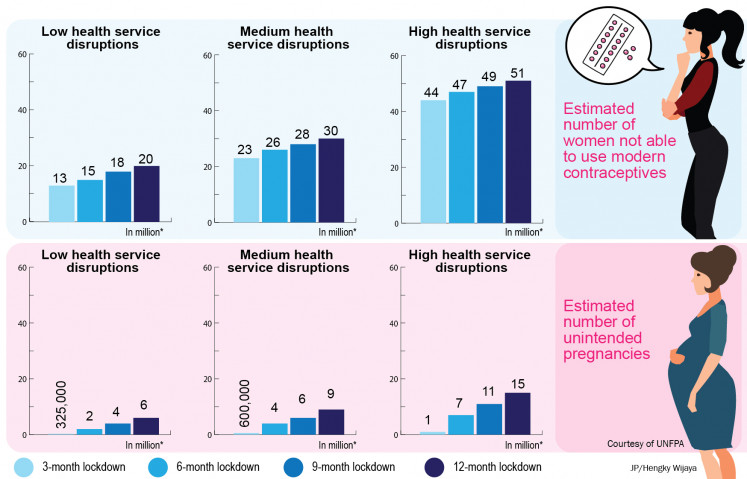
In need of attention: For every 3 months the lockdown continues, up to an additional 2 million women may be unable to use modern contraceptives. (Courtesy of UNFPA/-)Innovative financing and efforts for SRHR are crucial as the pandemic rages on, with an estimated 47 million women could lose access to contraception, leading to 7 million unintended pregnancies.
The data was released in April by the UNFPA, which is responsible for the United Nations’ sexual and reproductive health initiatives, based on research conducted in collaboration with Avenir Health, Johns Hopkins University and Victoria University in Australia.
The research shows the enormous impact COVID-19 is having on women as health systems become overloaded, facilities close or provide only limited services to women and girls and many people choose to skip important medical checkups because of fears of contracting the virus.
Global supply chain disruptions may also lead to significant shortages of contraceptives, and gender-based violence is expected to soar as women are trapped at home for prolonged periods.
“This new data shows the catastrophic impact that COVID-19 could soon have on women and girls globally. The pandemic is deepening inequalities, and millions more women and girls now risk losing the ability to plan their families and protect their bodies and their health,” said Natalia Kanem, UNFPA Executive Director.
“Women’s reproductive health and rights must be safeguarded at all costs. The services must continue; the supplies must be delivered; and the vulnerable must be protected and supported."
Unintended pregnancies may raise another problem – a baby boom – in countries like Indonesia, home to nearly 270 million people, which annually welcomes 4.8 million births.
Following the pandemic, the National Population and Family Planning Board (BKKBN) revealed in March that some 10 percent of its 28 million beneficiaries faced difficulty accessing birth control, and many clinics have shut while those that remain open have limited the number of people they serve.
The BKKBN estimated that a one-month decline in contraceptive use alone could push pregnancies up by 15 percent, or around 420,000 pregnancies, within three months.
In Bangladesh, Quazi AKM Mohiul Islam, former director general of family planning for the Health and Family Welfare Ministry, said that although the health system’s priorities had shifted to manage COVID-19, meeting the reproductive health needs of citizens was considered necessary as well.
“The lockdown has resulted in the close proximity of individuals and couples, increasing chances of sexual activity,” he said in his plenary presentation at the conference. “The Bangladesh government, development partners and the private sector are working together to strengthen coordination for contraceptive use during the pandemic.”
He said a National Preparation and Response Plan was being prepared that would take into account recent projections by the UNFPA regarding the increase of unintended pregnancies with the continuation of lockdowns and the issues of limited access to family planning services during the pandemic and of the complications that arose from the termination of pregnancy.
He said that sales of contraceptives, such as pills and condoms, from private pharmacies had increased. However, community distribution, house to house counselling and satellite sessions had been hampered.
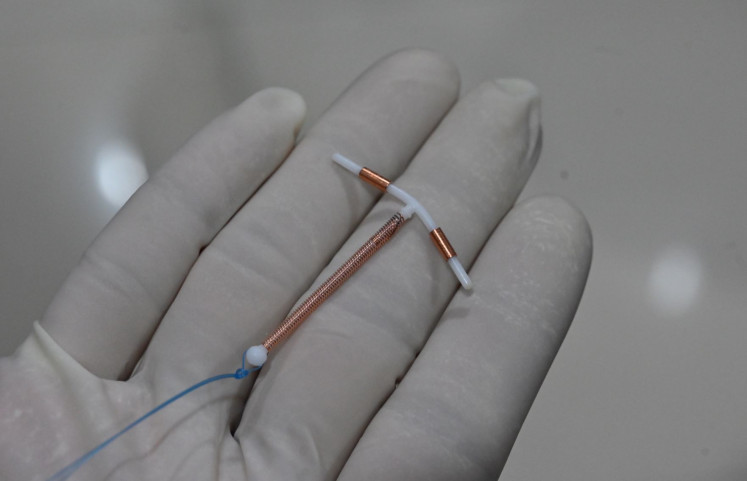
There has been a significant decrease in uptake of long-term reversible contraceptives, he said, but institutional deliveries followed by postpartum IUD, tubectomy and implants were continuing.
But there has been a decline in use of modern family planning methods as women are refraining from visiting health facilities due to fears about COVID-19 exposure or due to movement restrictions,” Mohiul said.
Up close: A doctor holds an IUD birth control device at a clinic in Jakarta. During the pandemic, some 10 percent of Indonesia’s 28 million family planning participants have faced problems accessing birth control. (AFP/Adek Berry)Angela Dawson, professor of public health at The Australian Centre for Public and Population Health Research, said many women around the world had experienced contraception failure, missed taking oral contraceptive pills or had been forced to have sex against their will.
For these women, she said, emergency contraception (EC) was a safe and effective method that reduced the risk of pregnancy.
She explained that EC, such as levonorgestrel, ulipristal and copper IUDs, could prevent more than 95 percent of pregnancies when taken within 5 days of intercourse and could be used after unprotected intercourse, to address concerns about possible contraceptive failure, after the incorrect use of contraceptives or after sexual assault.
However, many women remain unaware of this important option and in many countries in the Asia-Pacific region. Access to EC is still limited, and it remains a largely neglected contraceptive method.
Dawson said EC prevented pregnancy by preventing or delaying ovulation and that it was safe and effective – not an abortifacient and not teratogenic. “There is low knowledge, myths and misunderstandings, misinformation, stigma and discrimination around EC,” she said during the launch of the Asia Pacific Consortium for Emergency Contraception (APCEC) at the conference.
APCEC, which now has 11 member countries, aims to address these issues through advocacy efforts, teaching and networking to improve evidence-based policies and practice and access to EC.
Dawson said that during quarantines and lockdowns, rates of intimate partner violence appeared to have increased. Fear, health service closures and restricted hours due to staff redeployment had led to less access to EC and less uptake of regular contraception, increasing the likelihood of unintended pregnancy and possible contraceptive failure.
“All women and girls at risk of an unintended pregnancy have the right to access EC, and these methods should be routinely included within all national family planning programs. EC should be integrated into healthcare services for populations most at risk of exposure to unprotected sex,” she said.
“The need for EC is now more than ever.”